Expanding Access to Hemodialysis: Interview With an Expert in Home-Based Care
Home hemodialysis does have better outcomes because they are able to dialyze more frequently in shorter segments instead of having the big up-and-down spikes and constant blood pressure drop—and the toxins building up. -Ken Markovits, Hemodialysis Instructor at Clover Park Technical College (CPTC)
The rate of chronic kidney disease (CKD) in the U.S. may surprise you. It affects an estimated 37 million people in the U.S.—15 percent of the adult population. As the National Kidney Foundation describes it, CKD “is the under-recognized public health crisis” and is responsible for more deaths than breast cancer or prostate cancer.
Perhaps you don’t personally know of someone that has CKD, but you do likely know someone that has diabetes and high blood pressure, which are the top two causes of the disease. For some unlucky sufferers of these diseases, receiving dialysis becomes necessary to stay alive.
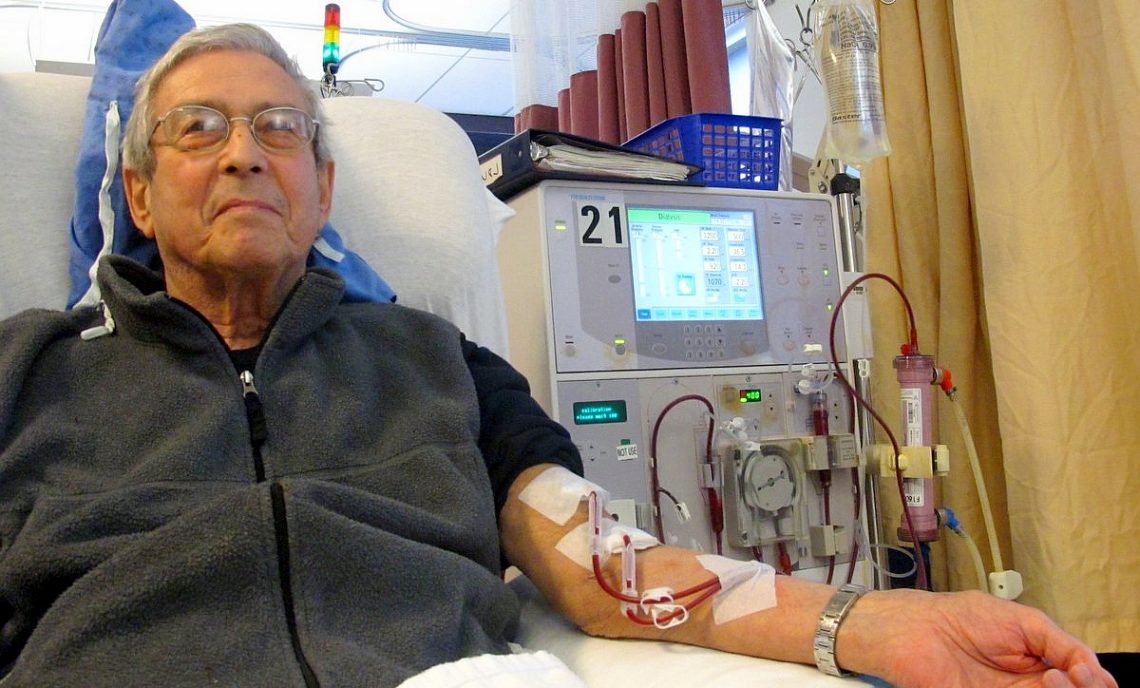
The treatment replaces the work of the patient’s malfunctioning kidneys, clearing waste and extra fluid from the blood in an external dialyzer, where it is cleaned and then returned to the patient’s body a little bit at a time. It’s a physically exhausting, time-consuming process that about half a million people in the U.S. go through each year.
Dialysis is not only physically taxing for patients—causing fatigue, nausea, body aches, and other symptoms—but can also take a psychological toll. Most patients end up spending three days a week at the hospital for four or five hours each time, which dramatically changes their daily routines.
Dialysis machines for home use have been around for the past few decades and have begun to become more prevalent in the last ten years. Performing the treatment at home can be a real game-changer for patients, by allowing them to maintain some control and normality in their schedules. Not only that, but studies also show that patients who choose the at-home option instead of the in-center option have better health outcomes. Surprisingly, only 10 percent of dialysis patients choose to take advantage of the at-home option. We talked to an expert to understand the full picture.
MEET THE INTERVIEWEE: HEMODIALYSIS EXPERT KEN MARKOVITS
Ken Markovits is a hemodialysis instructor at Clover Park Technical College (CPTC) in Washington state. Markovits was a student at CPTC in the program’s second class to go through the new program in 2003. He graduated in 2004, found work, and became a member of the program’s advisory board.
Markovits was hired as an adjunct faculty member and helped create the program curriculum. He continued to work in the industry while teaching until 2010. In 2015, Markovits was awarded tenure by CPTC’s board of trustees. Notably, in 2016, he was the chosen recipient of the National Institute for Staff and Organizational Development Excellence Award for his teaching at CPTC.
THE BENEFITS OF DIALYSIS AT HOME
“I’ve known patients that have done dialysis at home and they feel much better and the outcome is reflected in lab [results],” Ken Markovits said.
According to the National Kidney Foundation, benefits to patients who choose to do their hemodialysis treatments at home instead of in a medical center include:
- Less medication needed to control blood pressure and anemia
- Less medication needed to keep phosphorus under control to help prevent bone disease
- Improvements in neuropathy (nerve damage) and less restless leg syndrome
- Less fatigue and more energy for daily tasks
- Ability to sleep better
- Have fewer and shorter hospital stays
- Longer lifespan
WHAT IS HOME HEMODIALYSIS? WHY DOES IT IMPROVE PATIENT OUTCOMES?
For some dialysis patients, like those with acute kidney injury, treatment may just be used on a short-term basis to restore kidney function to normal. For other patients with more serious conditions, it’s a long-term treatment they must undergo while they wait to be matched with a donor for a kidney transplant.
Conventionally, dialysis is done three times a week for three- to four-hour periods. Because in-center dialysis is usually administered only three times a week per patient, there are days in between treatments in which the patient’s blood is not being cleaned.
Just as it sounds, home hemodialysis is similar to in-center hemodialysis treatment but done at the patient’s residence with the help of a care assistant, which can be a family member or friend who undergoes training with the help of a hemodialysis technician. Learning how to administer the treatment can take several weeks or a few months.
At the beginning of each treatment, two needles (which are connected to plastic tubing that carries blood to the dialyzer) are placed into the patient’s access. The dialysis machine pumps the patient’s blood through the dialysis system to cleanse it before it is returned to their body.
At home, it can be done more often in shorter increments (e.g. two-hour treatments, five to seven times a week). There’s also nocturnal home hemodialysis, which is done four to seven nights per week while the patient sleeps at night, for about six to eight hours. More hours of dialysis each week can result in more waste removal.
“Home hemodialysis does have better outcomes because they are able to dialyze more frequently in shorter segments instead of having the big up-and-down spikes and constant blood pressure drops—and the toxins building up,” Markovits said. “It keeps a more even keel doing home-hemo.”
More frequent, shorter sessions also means less of the patient’s blood needs to be removed each time, which can also drastically reduce side effects of dialysis like fatigue, headaches, and nausea.
The difference this makes for patients can be the “make or break” factor of whether or not an individual is able to continue their normal life. Some patients are even able to keep their regular jobs and daytime routines because of home hemodialysis, whereas in-center treatment usually makes that difficult or impossible.
WHY ISN’T HOME HEMODIALYSIS MORE POPULAR?
Despite the health, convenience, and lifestyle benefits of being able to perform dialysis treatments at home, the percentage of patients in the U.S. that undergo home hemodialysis is still very small. More than 90 percent of U.S. patients still choose conventional in-center hemodialysis.
Compared to other areas of the world, the U.S. is behind. “Most countries that currently have a pro-home-dialysis position tend to have around 30 to 40 percent [of patients doing home treatment],” Christopher Chan, MD, head of the division of nephrology at University Health Network (UHN) in Toronto told Medscape.
There are quite a few reasons that could be factoring into why the rate is still so low.
Some simply prefer to keep treatment and home life separate. “A lot of patients still want to go to the center because it might be their only social activity that they have that week. They know the people there; it’s an outing for them,” Markovits said. “Some of them feel like they’re already experiencing it 24 hours a day and don’t want to see [the equipment] 24 hours a day, too.”
Then, there are patients that just prefer being in the presence of a professional, who is trained in operating the equipment. “Some people may not want to jump into it because they may be afraid to be at home by themselves doing it, or even with a family member,” Markovits said.
It’s an understandable concern. Issues may arise with the machines, such as solution running out or air getting into the lines. In such a scenario, the patient would have to call their clinic and hopefully talk to a nurse who can help troubleshoot the problem.
“If it’s just a family member, they may not have all the answers,” he said. But, while learning how to operate the equipment may be intimidating at first, it’s do-able.
“It’s like driving a car. You don’t hop in a car and drive right away. You have somebody with you and you feel comfortable with that person and eventually, you feel comfortable enough to do it without them,” he said.
HOW CAN THE U.S. EXPAND ACCESS TO HOME-BASED HEMODIALYSIS?
Medicare covers training for self-dialysis with a technician and the costs of equipment and supplies. However, it does not cover the cost of having a technician continue to assist with treatments after training is completed.
“I know if I was a patient and I had the potential of having a technician that is trained there with me, I’d feel better,” Markovits said. “I’ve always said that if a dialysis company was smart about this, and they wanted to really get patients to do home-hemo, they should supply a technician for 60 to 90 days within [the patient’s] home.”
Of course, there is the reluctance of such companies to provide these services because of the extra cost. “I’ve tried to say that to higher-ups in the industry, and they jump on board in the moment, but nobody follows through. They can be a little stingy on that, but I think it would be an interesting option,” he added. Still, some patients opt to hire a technician to assist them for a short time, anyway.
A final factor preventing faster growth in home hemodialysis is the fact that even finding a center that offers it can be a challenge. Patients often have to research clinics in their area to inquire if they offer the service, but that is starting to change.
The U.S. government has begun to promote home hemodialysis since it is more cost-effective than in-center treatment (and therefore, reduces Medicare spending). It also increases the capacity in medical centers for those patients who are not good candidates for home hemodialysis.
In 2019, President Trump signed an executive order to launch Advancing American Kidney Health, an initiative, which in part, aims to promote patient welfare, but it will also curtail healthcare costs by promoting patients in the U.S. to opt for home dialysis. The initiative aims to have 80 percent of new patients with end-stage renal disease (ESRD) on home dialysis or receiving a transplant by 2025.
The nephrologist, Christopher Chan, said the 80 percent goal is “aspirational,” but hopes that it will jumpstart change—even if that goal is not met. “If someone is prepared and taught about home dialysis, they are much more likely to start,” he was quoted saying.
“On a personal note, if I were undergoing treatment, I would do it at home,” Markovits added. “The outcomes are better, and those spikes up and down are not going to be there . . . When a patient is more involved in the care, I think they tend to adhere more to medications and dietary restrictions and become healthier and feel better.”
This article originally appeared on the Medical Technology School website, and is reprinted here with permission from the author.
Share This Story
Ready to learn more? Visit the Hemodialysis program page on the Clover Park Technical College website.